Celebrate the holidays with WHYY!
Independence Blue Cross joins other insurance companies in restricting coverage of Wegovy and Ozempic to Type 2 diabetes and heart disease.
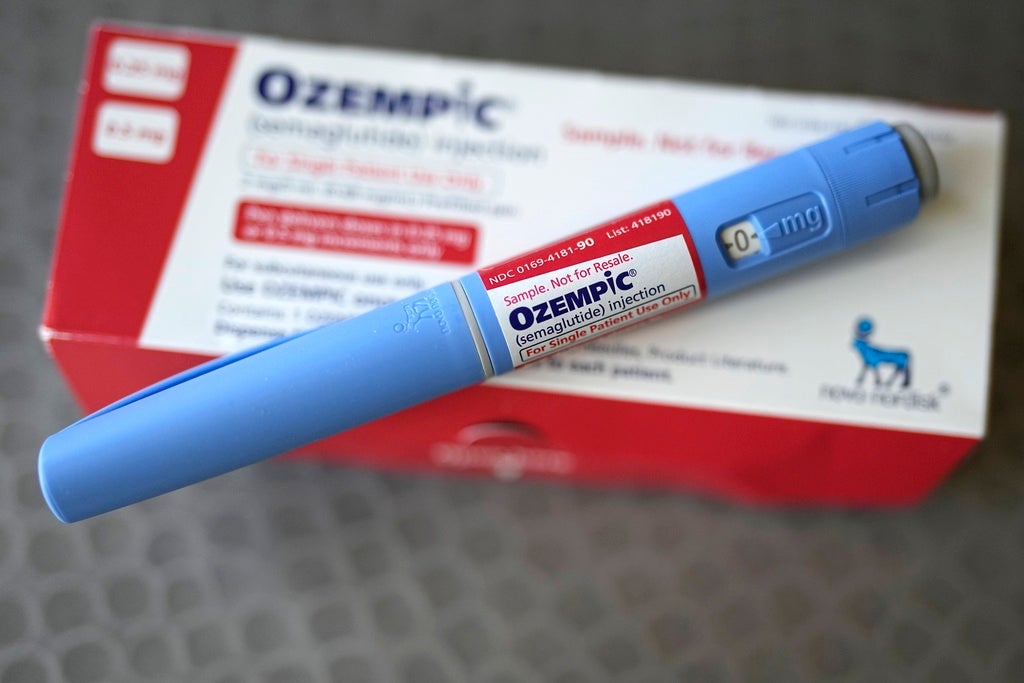
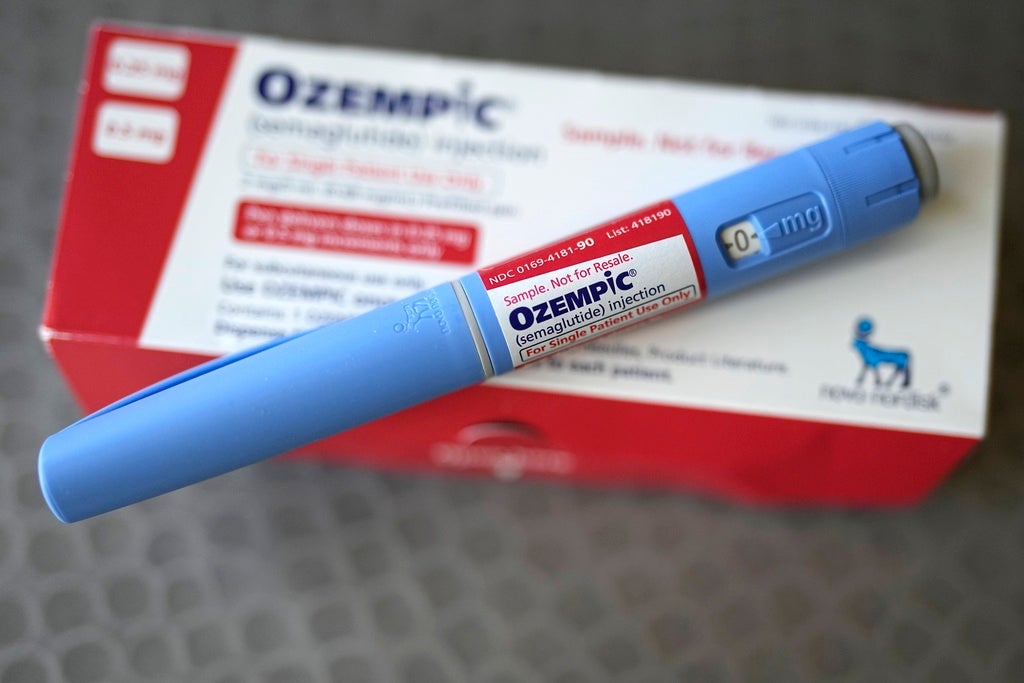
FILE – The injectable drug Ozempic is shown Saturday, July 1, 2023, in Houston. Even as millions of older adults clamor for drugs such as Ozempic and Wegovy, monthly use of the medications known as GLP-1 receptor agonists soared nearly 600% between 2020 and 2023 in people under 25 – and as young as 12. (AP Photo/David J. Phillip, File)
From Philly and the Pa. suburbs to South Jersey and Delaware, what would you like WHYY News to cover? Let us know!
The popularity of medications like Wegovy, Ozempic, Mounjaro and Zepbound for weight loss and obesity has skyrocketed in recent years, with both patients and health providers citing successful outcomes with continued use.
But the sticker prices of these injectable drugs remain expensive – about $700 to $1,350 for a month’s supply at the highest – and the costs have fallen on patients and their insurance providers.
While there are some state and federal efforts to expand insurance coverage for these drugs in public programs like Medicaid and Medicare, some local private insurers like Independence Blue Cross (IBX) are restricting coverage.
Beginning Jan. 1, people with IBX health plans will have to pay the full cost of GPL-1 agonists and other similar drugs when they are prescribed solely for weight loss.
IBX, the largest insurer in southeastern Pennsylvania, will continue to cover these medications when they are prescribed for people with conditions approved by the Food and Drug Administration, such as Type 2 diabetes and cardiovascular disease.
People who get insurance through their employers may still get coverage if the individual companies or organizations decide to include weight loss drugs in their prescription plans.
In a Nov. 1 notice to health plan members, IBX said the decision “was not made lightly” and that continued coverage of these high-priced drugs could lead to increased premiums for everyone else.
“These exorbitant costs have made it extremely challenging to be able to continue to provide drug coverage to everyone who wants these drugs but does not have an FDA-approved medical or indication for these drugs,” the company stated.
Other major insurance companies and large employers have similarly restricted or dropped coverage, including Blue Cross Blue Shield of Michigan, North Carolina’s State Health Plan, RWJBarnabas Health in New Jersey, the Mayo Clinic and Ascension.
Pennsylvania is among a small number of states that cover these medications for obesity, in addition to Type 2 diabetes, through its Medicaid program, but the cost to do so remains high. The state spent nearly $298 million, or about $106 per enrollee, for these drugs from November 2023 to this past October, according to new data from Real Chemistry.
Wegovy works. But here’s what happens if you can’t afford to keep taking the drug
There’s been such an increase in demand that an FDA database lists the medication’s active ingredient, semaglutide, as “currently in shortage.”
2 years ago
The list prices for these weight loss medications is an ongoing problem that needs to be addressed, said Dr. Kunal Shah, clinical director of obesity medicine at the Rutgers Center for Metabolic Health and Weight Management.
But he said there is potential for long-term savings if people can use these medications to better manage or prevent risks and complications related to obesity, including heart disease, diabetes, cancer, kidney disease, osteoarthritis, asthma and more.
Shah said there are some people who want these medications not because they are obese or overweight, but rather to become even thinner or reach a specific lower weight.
But broadly reducing access to these drugs through insurance restrictions and cuts will likely affect many more people whose weight is causing them health issues and affecting their quality of life, he said.
“I’ll have someone who has pre-diabetes, who has sleep apnea, who has COPD and they’re 300, 400 pounds. They’re on oxygen, they can barely get up out of their seat without getting short of breath,” Shah said. “Losing 30, 40, 50, 60 ,70, even 100 pounds would be life changing. They may be able to get off oxygen, they may be able to exercise more. And then I have to tell them, listen, your insurance is not going to cover it.”
Shah said this can be an especially frustrating situation for patients who are older and may not have the physical ability to exercise as much as they once did, so medication for weight loss could be an alternative option.
But Medicare, which is a federal insurance program for people 65 and older, does not cover these medications solely for weight management, only for diabetes and heart disease.
“Part of the difficulty with being a physician that treats medical obesity is having to come up with options that we know are not superior to what we want to give and having to give ‘inferior’ options because the limiting factor is insurance coverage,” Shah said.
How Ozempic is changing weight loss
GLP-1s like Ozempic and Mounjaro are wildly popular for treating diabetes, obesity and now cosmetic weight-loss. How are they changing health care and our culture?
Air Date: September 19, 2024 12:00 pm
Ahead of changes in 2025, Shah said there are some things people can do in anticipation of losing insurance coverage for these medications.
He recommends that patients who currently have a prescription for a GPL-1 or other type of weight loss drug ask their health providers for a three-month refill now, “so that gives you some time in case you do need to pivot.”
For people who may be newly considering weight loss medications in the new year, Shah said they should get evaluated by health providers who specialize in obesity medicine, because if they identify conditions like Type 2 diabetes or cardiovascular disease, there’s a better chance that insurance will cover medications.
There are other weight management and obesity treatment options available to people, Shah said, including different types of medications that may or may not be as effective as some of the GPL-1 drugs.
Insurance providers, including Independence Blue Cross, continue to cover nutrition and behavioral health counseling, incentive programs for fitness and exercise activities and bariatric surgery for people at risk of becoming obese.
The WHYY health desk is expanding coverage of weight management and obesity challenges. To share a personal experience or story idea, email reporter Nicole Leonard at nleonard@whyy.org.
Get daily updates from WHYY News!
The free WHYY News Daily newsletter delivers the most important local stories to your inbox.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
Americans are furious over health care. Is this an Occupy Wall Street moment?
The public outrage unleashed by the killing of UnitedHealthcare’s CEO echoes the anti-banking fury after the financial crisis.
1 week ago
New Jersey is considering banning sales of diet and muscle building pills to minors
This comes after a similar law went into effect in New York — the first in the country.
2 weeks ago
Philadelphia nurse and patient advocate to testify before the U.S. Department of Labor on fighting insurance denials
Nearly 1 in 5 people say they’ve experienced a health insurance denial within the past year, according to a national survey.
3 months ago
Nicole Leonard is a health and science reporter for WHYY News.
3 hours ago
3 hours ago
4 hours ago
Want a digest of WHYY’s programs, events & stories? Sign up for our weekly newsletter.
Together we can reach 100% of WHYY’s fiscal year goal
WHYY provides trustworthy, fact-based, local news and information and world-class entertainment to everyone in our community.
WHYY offers a voice to those not heard, a platform to share everyone’s stories, a foundation to empower early and lifelong learners and a trusted space for unbiased news. Learn more about Social Responsibility at WHYY. It’s how we live.
215.351.1200
talkback@whyy.org
302.516.7506
talkback@whyy.org
© MMXXIV WHYY
WHYY is partnered with
source