Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
Advertisement
Scientific Reports volume 15, Article number: 857 (2025)
Metrics details
This study aimed to explore the relationship between the lymphocyte/monocyte ratio (LMR) and erectile dysfunction (ED) in adult men in the United States using a comprehensive dataset. A cross-sectional study design was used to analyze the relationship between the lymphocyte-to-monocyte ratio (LMR) and the prevalence of erectile dysfunction (ED) among adult male participants in the NHANES 2001–2004 dataset. Statistical analyses were performed to adjust for potential confounders and explore non-linear associations, with LMR categorized into quartiles to investigate the relationship with ED prevalence. There was an L-shaped relationship between LMR and ED. The odds of ED decreased as LMR levels increased, but beyond a value of 3.50, the protective effect plateaued. Specifically, the odds of ED significantly decreased for LMR values ≤ 3.50 (OR = 0.67, 95% CI: 0.49–0.90, p = 0.009). Beyond an LMR of 3.50, there was no significant further reduction in the odds of ED, indicating a diminishing protective effect past this threshold. There is a distinctly L-shaped and negative correlation between LMR and ED in the NHANES dataset from 2001 to 2004.
Erectile Dysfunction (ED) is a significant health issue that substantially affects the psychosocial health of men. The prevalence of ED among young men is as high as 30%1, with an increasing trend in incidence rates year by year. The etiology of ED is complex, encompassing vascular, neurogenic, endocrinologic, and psychogenic factors2. ED often precedes cardiovascular diseases (CVD)3, sharing mechanisms such as endothelial dysfunction and chronic inflammation, both of which contribute to disease progression4.
Pro-inflammatory molecules such as IL-6, VCAM-1, and MCP-1 impair endothelial function by reducing NO bioavailability, which promotes vascular dysfunction5. Monocytes are one of the major sources of these inflammatory mediators, and their activation amplifies endothelial injury through cytokine secretion and adhesion to the vascular endothelium6. In contrast, lymphocytes, particularly regulatory T cells, are critical in maintaining immune balance and vascular homeostasis7. A decrease in the lymphocyte-to-monocyte ratio (LMR) indicates a shift toward a pro-inflammatory state, marked by increased monocyte activity and reduced lymphocyte-mediated regulation. These inflammatory pathways not only contribute to the development of erectile dysfunction (ED), but also highlight the need for reliable biomarkers to assess systemic inflammation and its impact on disease progression.
The lymphocyte-to-monocyte ratio (LMR) is an emerging biomarker reflecting systemic inflammation and has been extensively studied in the context of cardiovascular diseases. Lower LMR levels have been associated with more severe coronary atherosclerosis8, highlighting its potential as a predictor of vascular health.Given the shared inflammatory and vascular mechanisms between CVD and ED, we hypothesize that lower LMR levels may increase ED risk.However, the relationship between LMR levels and ED has not been reported. Therefore, this study aims to investigate the association between LMR levels and the occurrence of ED using a large database to incorporate more comprehensive data, with the goal of early identification and intervention of ED progression, and to explore valuable biomarkers. We aim to utilize the lymphocyte-to-monocyte ratio (LMR) as an early predictor.This approach could enable early intervention to reduce adverse events and support personalized treatment plans for patients with erectile dysfunction.Future studies could further explore the association of LMR with ED and other genitourinary diseases, such as prostatitis or urinary tract infection, to expand the application of this biomarkers.
This is a cross-sectional study based on data from the National Health and Nutrition Examination Survey (NHANES), a research program designed to assess the health and nutritional status of adults and children in the United States, focusing on various health and nutrition measurements to meet emerging needs. In this study, we collected data from two NHANES cycles (2001–2002 and 2003–2004), with more information about the data available on the NHANES website (www.cdc.gov/nchs/nhanes/).
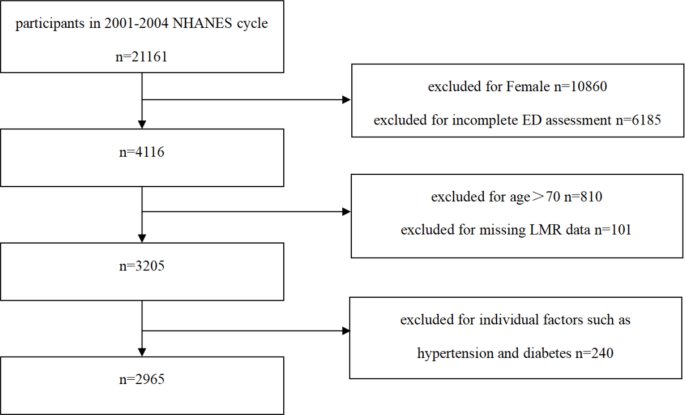
In this cross-sectional study, data from the two survey cycles (2001–2002 and 2003–2004) were used because information on erectile dysfunction (ED) was only available during the period from 2001 to 2004. This survey period was chosen as ED data were pertinent to these cycles. Within this timeframe, NHANES had a total of 21,161 relevant records. After excluding females (n = 10,860) because ED is a male-specific condition, individuals with missing ED-related data (n = 6,185) or leukocyte data (n = 101) were excluded, as the latter prevented the calculation of the lymphocyte-to-monocyte ratio (LMR), ensuring data completeness and analytical consistency. Participants aged over 70 years (n = 810) were excluded to minimize potential confounding from age-related health conditions. Additionally, participants with missing data on PIR, hypertension, or diabetes (n = 240) were excluded, as these variables are critical for model adjustment. Including participants with incomplete data on these variables could have introduced bias and reduced the robustness of the regression models. The exclusion of individuals with missing data for hypertension and diabetes, although necessitated by data incompleteness, may introduce selection bias. This limitation is acknowledged in the Discussion section.The study ultimately included 2,965 participants, comprising 2419 individuals with ED and 546 without ED (Fig. 1)
Flow chart of the study.
The lymphocyte-to-monocyte ratio (LMR) is an index that can effectively reflect the inflammatory status of a patient, calculated by dividing the peripheral blood lymphocyte count by the monocyte count. The lymphocyte and monocyte counts are analyzed through complete blood cell counts using the Beckman Coulter automatic analyzer. The detailed analytical procedures are described in Laboratory/Medical Technologists Procedures Manual (https://wwwn.cdc.gov/nchs/nhanes/). In terms of assessing erectile dysfunction (ED), Many men often encounter difficulties expressing problems related to sexual function. Erectile dysfunction (ED) was assessed using a self-administered questionnaire. Participants were asked the following question: “How would you describe your ability to obtain and maintain an erection to reach satisfactory sexual activity?” The possible answers included: (1) always or almost always able to get and keep an erection, (2) usually able to get and keep an erection, (3) sometimes able to get and keep an erection, and (4) never able to get and keep an erection. Individuals who selected “never” or “sometimes” were classified as having ED.
Age is a major risk factor for ED, as the risk increases with age. Ethnicity and marital status may also influence the incidence of ED through socioeconomic or psychological factors. Hypertension and diabetes are known to affect vascular function and are directly associated with ED. Therefore, covariates such as age, ethnicity, marital status, Poverty Income Ratio (PIR), history of diabetes, and history of hypertension were analyzed. Ethnicity was categorized into Mexican American, non-Hispanic white, non-Hispanic black, other Hispanic, and other ethnicitiess. The Poverty Income Ratio (PIR) is an index of household income relative to poverty, reflecting socioeconomic status. The Poverty Income Ratio (PIR) is an index used to measure socioeconomic status, with specific cut-off values defined by guidelines published annually by the Department of Health and Human Services (HHS). According to these guidelines, PIR is categorized into three groups: ≤ 1.3, 1.3 < PIR ≤ 3.5, and > 3.5. PIR reflects socioeconomic factors such as access to healthcare, nutrition, and lifestyle, which are known to influence the risk of ED9,10. Lower PIR values are associated with limited access to resources, which may exacerbate risk factors for ED, such as chronic diseases and poor psychological well-being11. Ethnicity and marital status may also influence the incidence of ED through socioeconomic or psychological factors12. Marital status may affect ED risk by influencing emotional and psychological stability. Studies suggest that married individuals tend to report better sexual and mental health outcomes13, which are protective factors against ED. These covariates are considered potential confounding factors that could influence the relationship between LMR and ED and were included in the multivariate model.
The LMR was categorized into quartiles Q1 (≤ 2.93), Q2 (2.93,3.71), Q3 (3.71, 4.57), Q4( ≥ 4.57), respectively. The lymphocyte-to-monocyte ratio (LMR) was categorized into quartiles to allow for the exploration of non-linear associations between LMR and erectile dysfunction (ED). Quartile-based categorization is a commonly used approach in epidemiological studies, as it facilitates comparison across subgroups and minimizes the influence of extreme values. The thresholds were determined based on the distribution of LMR values in the study population and were aligned with prior studies investigating inflammatory biomarkers14. Continuous variables were expressed as mean ± standard deviation (SD) if normally distributed or median (IQR) if not, while categorical variables were presented as frequency counts and proportions (n, %). Normality of continuous variables was assessed using the Shapiro-Wilk test. The Chi-square (χ²) test was employed for categorical variables, and one-way Analysis of Variance (ANOVA) was used for normally distributed continuous variables to test for differences across LMR quartiles. Results are reported in Table 1. No covariables were adjusted in Model 1. Model 2 was adjusted for age、ethnicity and marital status and model 3 for all covariates from Table 1 except ED. A two-sided p-value of < 0.05 was considered statistically significant. All statistical analyses were conducted using EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc.) and statistical software packages R (http://www.R-project.org; The R Foundation).
A total of 2,965 participants participated in our study, including 2,419 ED patients and 546 participants without ED. LMR levels were higher in non-ED patients (3.73 (95%CI: 3.67, 3.78)compared with those ED patients (3.53 (95%CI: 3.41,3.65),p = 0.001.Patients with ED were older, married or living with a partner, had diabetes, high blood pressure, and Table 1 lists the detailed demographics of all the surveyors.
Univariate logistic regression was performed to evaluate the association between LMR and all selected covariates and ED, as shown in Table 2 In addition, we converted continuous variable LMR into categorical variable by quartile and used multivariate logistic regression to test the relationship between LMR and ED in rough, minimum adjusted and fully adjusted models.It was found that there was a significant negative correlation between LMR and ED in the four categories in the fully adjusted model, with statistical significance. Compared with the respondents in the lowest quartile (Q1), the risk of ED among the respondents in the highest quartile (Q4) was reduced by 26.7% (OR = 0.743,95%CI: Compared with Q1, the OR(95%CI) of Q2, Q3 and Q4 participants were 0.698(0.520, 0.936), 0.666(0.491,0.903) and 0.743(0.552,0.999), respectively, as shown in Table 3. Figure 2 shows a non-linear relationship plot between Lymphocyte-to-Monocyte Ratio (LMR) and Erectile Dysfunction (ED), with an L-shaped association. The blue line represents the 95% confidence interval for the fitted values, while the red line represents the predicted probability of ED based on LMR. An inflection point at LMR of approximately 3.5 is observed, indicating the change in the risk of ED as LMR increases.
Non-linear relationship plot between LMR and ED. The red line represents the predicted probability of erectile dysfunction (ED) based on the lymphocyte-to-monocyte ratio (LMR). The blue line represents the 95% confidence interval for the predicted probability.
After adjusting for the relevant covariates (all covariates except LMR in Table 1), we analyzed the interactions and subgroup analyses between LMR and ED.In subgroup analyses stratified by age, ethnicity, history of hypertension, history of diabetes, there was no significant interaction.At the same time, our results show a negative correlation between LMR levels and ED in most subgroups, although this was not evident in the cross-test (Fig. 3).
Subgroup analysis. Subgroup-specific odds ratios (ORs) and 95% confidence intervals (CIs) are shown for quartile-based LMR analysis. Sample sizes for each subgroup are as follows: Age: ≤50 years (n = 1946), > 50 years (n = 1019). Hypertension: Yes (n = 635), No (n = 2330). Diabetes: Yes (n = 168), No (n = 2797). Ethnicity: White (n = 1529), Non-white (n = 1436).
In this cross-sectional study, we investigated the connection between the Lymphocyte-to-Monocyte Ratio (LMR) and Erectile Dysfunction (ED), finding that after adjusting for related confounding factors, LMR is inversely and L-shaped associated with ED.Our findings suggest that LMR is a potential biomarker for assessing ED risk. This interpretation aligns with prior studies linking LMR to systemic inflammation and endothelial dysfunction, both key contributors to ED. For instance, Yang et al. reported that a lower LMR was an independent predictor of coronary slow flow (CSF) in isolated coronary artery ectasia (CAE), highlighting its association with heightened inflammation and vascular dysfunction15. These mechanisms are relevant to ED pathophysiology and suggest that LMR may reflect underlying vascular health. Although our study is based on a cross-sectional population from NHANES, the observed association may be generalizable to populations with similar health profiles. Future research should validate this finding in diverse populations and investigate its clinical utility.
Erectile Dysfunction (ED) is a disease that leads to male sexual dysfunction. Its etiology is complex, and studies have shown that the incidence of diabetes in patients with ED is 3–5 times higher than in those without ED16. ED could be an early marker17of latent endocrine disorders and is also an independent predictor of cardiovascular diseases (CVD)18, aligning with our study’s findings that the ED population has a higher probability of comorbidities like hypertension and diabetes. Numerous studies indicate that inflammation-induced endothelial dysfunction is a fundamental pathophysiological symptom of ED, and the development and degree of ED have been proven to be related to markers of inflammation and endothelial dysfunction, such as high-sensitivity C-reactive protein19. Such inflammatory indicators may better monitor the occurrence of ED.
LMR is a convenient and low-cost biomarker, showing superiority in predicting endothelial dysfunction-induced CVD over individual monocyte counts or lymphocyte levels alone20. LMR has been effective in diagnosing and determining the prognosis of inflammatory diseases and malignancies21. LMR (OR, 0.680; 95%CI 0.560–0.825, P = 0.001) is an independent factor for early neurologic deterioration (END) after thrombolysis22. In patients with ulcerative colitis, a significant elevation of LMR was observed in the active UC group compared to inactive UC and controls23. In various urinary and other systemic cancers, LMR is also associated with a favorable prognosis24,25.
The relationship between LMR and ED has been explored in only a limited number of studies, and the findings have been inconsistent. In a study investigating the effect of daily tadalafil on Index of Erectile Function-5(IIEF-5) scores, LMR, and MHR, an approximate 8-point increase in IIEF-5 scores was observed in the ED group after 8 weeks of tadalafil (p = 0.001), The IIEF-5 is a standardized questionnaire widely used to assess erectile function, with higher scores indicating better erectile function26,but no significant differences were found in LMR and MHR before and after treatment or compared to the control group27. Yet, another study showed LMR to be a statistically significant predictor in univariate analysis28. Discrepancies may stem from differences in study design, sample size, and population characteristics. Our dataset, based on a large, nationally representative sample, offers broader generalizability compared to prior studies with smaller, localized cohorts. Variations in baseline inflammation, comorbid conditions (e.g., hypertension, diabetes), and socioeconomic factors could also influence the observed associations.
While our study highlights LMR as a potential biomarker for ED risk, its predictive utility may vary with clinical context. For example, as suggested by the tadalafil study, LMR might be less sensitive to short-term pharmacological changes but more reflective of long-term systemic inflammation and vascular health.
In our study, we divided patients’ LMR into quartiles and found that the Q3 group demonstrated the most significant protective effect. This approach allowed us to observe an L-shaped association between LMR and ED, which may not have been detected in studies employing linear models or smaller sample sizes. Although the likelihood of ED generally decreases with increasing LMR levels, our findings suggest a threshold effect, with the protective effect diminishing beyond an LMR value of 3.5. This observation highlights the potential importance of considering non-linear associations when evaluating biomarkers, though further studies are needed to confirm this finding.
The underlying mechanism of this L-shaped association may involve inflammatory pathways and oxidative stress. Monocytes, which secrete pro-inflammatory cytokines like interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), contribute to endothelial dysfunction by depleting nitric oxide (NO), thereby impairing vasodilation29. In contrast, regulatory T cells modulate inflammation and maintain vascular homeostasis30. Excessive reactive oxygen species (ROS) exacerbate endothelial damage by reducing NO bioavailability and increasing vascular permeability31. The observed threshold effect in the LMR-ED relationship may reflect a delicate balance between pro-inflammatory and anti-inflammatory processes. At low LMR levels, heightened inflammation may contribute to endothelial dysfunction, whereas elevated LMR levels could indicate immune dysregulation, potentially leading to excessive oxidative stress.
This study has several strengths. First, we used a nationally representative sample of ED adults in the United States, which is relatively large and helps generalize our results. Second, by adjusting for socioeconomic status, ethnicity, previous disease factors, and other potential confounding factors, we could enhance the validity of our conclusions. Lastly, LMR levels in the NHANES database were measured using standardized methods, ensuring the reliability of data analysis.
Furthermore, the L-shaped association between LMR and ED observed in this study may be helpful for early screening and treatment of ED patients. For instance, patients with lower LMR levels may require more aggressive interventions to reduce the risk of developing ED. This finding provides a basis for personalized treatment plans, allowing for different therapeutic strategies based on LMR levels, especially those focusing on reducing inflammation or improving immune function. Future research could explore the efficacy of LMR as a predictive marker for ED and evaluate its performance across different populations. Additionally, further studies should investigate the relationship between LMR and other biomarkers, as well as their impact on ED and other urological diseases.
Our study also has some limitations.First, due to its cross-sectional design, it does not allow for causal inferences.Second, potential selection bias may have occurred because individuals with missing data were excluded from the analysis. Specifically, the exclusion of participants with missing data on hypertension and diabetes, although necessary to maintain data consistency, might have led to the underrepresentation of individuals with these known risk factors for ED, potentially underestimating the true association between LMR and ED. However, hypertension and diabetes were included as covariates in our fully adjusted model, which mitigates some of this bias.Certain subgroups, such as participants with diabetes, have relatively small sample sizes, which might limit the statistical power and reduce the generalizability of the findings. Despite this, the overall trends observed across subgroups remain consistent, supporting the robustness of our conclusions.Third, LMR data was derived from single blood tests, which may not fully capture chronic inflammatory status. Lastly, as the study population was primarily American, the findings may not be generalizable to other ethnicities. Larger multi-ethnic studies with repeated measures of LMR would provide a more comprehensive understanding of its association with ED.And future research should explore the mechanisms linking LMR to ED, particularly in relation to inflammation, vascular dysfunction, and endothelial health. Investigating these mechanistic pathways will help clarify how LMR functions as a potential biomarker and therapeutic target. Additionally, longitudinal studies are essential to validate these findings and explore the causal relationship between LMR and ED.In light of our findings, future research could consider investigating the potential of LMR as a therapeutic target for ED, which may offer valuable insights for clinical applications.
Our study demonstrates a significant L-shaped association between LMR and ED, supporting its potential as a biomarker. Further longitudinal and mechanistic studies are warranted to confirm these findings and explore their clinical relevance.
The datasets analysed during the current study are available in the NHANES repository(NHANES – National Health and Nutrition Examination Survey Homepage (cdc.gov).
Nguyen, H. M. T., Gabrielson, A. T. & Hellstrom, W. J. G. Erectile dysfunction in young men-A review of the prevalence and risk factors. Sex. Med. Rev. 5 (4), 508–520. https://doi.org/10.1016/j.sxmr.2017.05.004 (2017).
Article PubMed Google Scholar
MacDonald, S. M. & Burnett, A. L. Physiology of erection and pathophysiology of erectile dysfunction. Urol. Clin. N. Am. 48 (4), 513–525. https://doi.org/10.1016/j.ucl.2021.06.009 (2021).
Article Google Scholar
Orimoloye, O. A., Feldman, D. I. & Blaha, M. J. Erectile dysfunction links to cardiovascular disease-defining the clinical value. Trends Cardiovasc. Med. 29 (8), 458–465. https://doi.org/10.1016/j.tcm (2019).
Article PubMed Google Scholar
Kaya-Sezginer, E. & Gur, S. The inflammation network in the pathogenesis of erectile dysfunction: attractive potential therapeutic targets. Curr. Pharm. Des. 26 (32), 3955–3972. https://doi.org/10.2174/1381612826666200424161018 (2020).
Article CAS PubMed Google Scholar
Hartge, M. M., Unger, T. & Kintscher, U. The endothelium and vascular inflammation in diabetes. Diab. Vasc. Dis. Res. 4 (2), 84–88. https://doi.org/10.3132/dvdr.2007.025 (2007).
Article PubMed Google Scholar
Libby, P., Ridker, P. M. & Hansson, G. K. Progress and challenges in translating the biology of atherosclerosis. Nature 473 (7347), 317–325. https://doi.org/10.1038/nature10146 (2011).
Article ADS CAS PubMed Google Scholar
Sakaguchi, S., Yamaguchi, T., Nomura, T. & Ono, M. Regulatory T cells and immune tolerance. Cell 133 (5), 775–787. https://doi.org/10.1016/j.cell.2008.05.009 (2008).
Article CAS PubMed Google Scholar
Kaya-Sezginer, E. & Gur, S. The inflammation network in the pathogenesis of erectile dysfunction: attractive potential therapeutic targets. Curr. Pharm. Des. 26 (32), 3955–3972. https://doi.org/10.2174/1381612826666200424161018 (2020).
Article CAS PubMed Google Scholar
Yogeswaran, V. et al. Association of poverty-income ratio with cardiovascular disease and mortality in cancer survivors in the United States. PLoS One 19(7), e0300154. https://doi.org/10.1371/journal.pone.0300154 (2024).
Macdonald, E. J., Gaines, J. M. & Kim, J. I. Exploring the Relationship between Socioeconomic Status and Erectile Dysfunction: An Analysis of the National Health and Nutrition Examination Survey (International Journal of Impotence Research, 2023).
Fang, Y. et al. The role of Socioeconomic Status and Oxidative Balance Score in Erectile Dysfunction: A cross-sectional Study (Heliyon, 2023).
Kupelian, V., Link, C. L., Rosen, R. C. & McKinlay, J. B. Socioeconomic status, not race/ethnicity, contributes to variation in the prevalence of erectile dysfunction: results from the Boston Area Community Health (BACH) Survey. J. Sex. Med. 5 (6), 1325–1333. https://doi.org/10.1111/j.1743-6109.2008.00822.x (2008).
Article PubMed Google Scholar
Kravdal, Ø., Wörn, J. & Reme, B. A. Mental health benefits of cohabitation and marriage: a longitudinal analysis of Norwegian register data. Popul. Stud. (Camb.) 77 (1), 91–110. https://doi.org/10.1080/00324728.2022.2063933 (2023).
Article PubMed Google Scholar
Hu, X. et al. Association between preoperative lymphocyte-to-monocyte ratio and occurrence of postoperative cognitive dysfunction: a prospective cohort study. J. Inflamm. Res. 17, 9527–9537. https://doi.org/10.2147/JIR.S481106 (2024).
Article PubMed PubMed Central Google Scholar
Yang, Z., Yuan, J., Cui, J., Guan, H. & Qiao, S. Association of the lymphocyte-to-monocyte ratio, mean diameter of coronary arteries, and uric acid level with coronary slow flow in isolated coronary artery ectasia. BMC Cardiovasc. Disord. 21(1), 156. https://doi.org/10.1186/s12872-021-01952-4 (2021).
Xiang, Q., Liu, Y., Xiao, J., Ou, L. & Du, J. Prognostic value of lymphocyte-to-monocyte ratio (LMR) in patients with prostate cancer: a systematic review and meta-analysis. Am. J. Mens Health. 18 (2), 15579883241234747. https://doi.org/10.1177/15579883241234747 (2024).
Article PubMed PubMed Central Google Scholar
Defeudis, G. et al. Erectile dysfunction and diabetes: a melting pot of circumstances and treatments. Diabetes Metab. Res. Rev. 38 (2), e3494. https://doi.org/10.1002/dmrr.3494 (2022).
Article PubMed Google Scholar
Mazzilli, R. et al. Erectile dysfunction as a marker of endocrine and glycemic disorders. J. Endocrinol. Invest. 45 (8), 1527–1534. https://doi.org/10.1007/s40618-022-01788-5 (2022).
Article CAS PubMed PubMed Central Google Scholar
Mostafaei, H. et al. Association of erectile dysfunction and cardiovascular disease: an umbrella review of systematic reviews and meta-analyses. BJU Int. 128 (1), 3–11. https://doi.org/10.1111/bju.15313 (2021).
Article PubMed PubMed Central Google Scholar
Liu, G. et al. Novel predictive risk factor for erectile dysfunction: serum high-sensitivity C-reactive protein. Andrology 10 (6), 1096–1106. https://doi.org/10.1111/andr.13206 (2022).
Article CAS PubMed Google Scholar
Kumarasamy, C. et al. Prognostic significance of blood inflammatory biomarkers NLR, PLR, and LMR in cancer-A protocol for systematic review and meta-analysis. Medicine (Baltimore) 98 (24), e14834. https://doi.org/10.1097/MD.0000000000014834 (2019).
Article PubMed Google Scholar
Gong, P. et al. The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J. Neuroinflamm. 18(1), 51. https://doi.org/10.1186/s12974-021-02090-6 (2021).
Li, J. et al. Association between multiple inflammatory biomarkers and remnant cholesterol levels in patients with percutaneous coronary intervention: a large-scale real-world study. Nutr. Metab. Cardiovasc. Dis. 34 (2), 377–386. https://doi.org/10.1016/j.numecd.2023.09.006 (2024).
Article CAS PubMed Google Scholar
Zhang, L. et al. Meta-analysis of multiple hematological biomarkers as prognostic predictors of survival in bladder cancer. Medicine (Baltimore) 99 (30), e20920. https://doi.org/10.1097/MD.0000000000020920 (2020).
Article CAS PubMed Google Scholar
Xiang, Q., Liu, Y., Xiao, J., Ou, L. & Du, J. Prognostic value of lymphocyte-to-monocyte ratio (LMR) in patients with prostate cancer: a systematic review and meta-analysis. Am. J. Mens Health 18 (2), 15579883241234747. https://doi.org/10.1177/15579883241234747 (2024).
Article PubMed PubMed Central Google Scholar
Neijenhuijs, K. I. et al. The International Index of Erectile function (IIEF)-A systematic review of measurement properties. J. Sex. Med. 16 (7), 1078–1091. https://doi.org/10.1016/j.jsxm.2019.04.010 (2019).
Article PubMed Google Scholar
Mercimek, M. N., Kolukcu, E. & Bostanci, Y. Does tadalafil 5 mg/day affect lymphocyte to monocyte and monocyte to high-density lipoprotein ratios in patients with erectile dysfunction? Ann. Med. Res. 27, 2340–2345 (2020).
Article Google Scholar
Kilic, M., Erkan, A., Zengin, S., Dundar, G. & Boyaci, C. Inflammatory biomarkers may predict response to phosphodiesterase type 5 inhibitor treatment in patients with erectile dysfunction. Investig. Clin. Urol. 64 (4), 404–411. https://doi.org/10.4111/icu.20230013 (2023).
Article PubMed PubMed Central Google Scholar
Yasmeen, F., Pirzada, R. H., Ahmad, B., Choi, B. & Choi, S. Understanding autoimmunity: Mechanisms, predisposing factors, and cytokine therapies. Int. J. Mol. Sci. 25(14), 7666. https://doi.org/10.3390/ijms25147666 (2024).
Calmasini, F. B., Klee, N., Webb, R. C. & Priviero, F. Impact of immune system activation and vascular impairment on male and female sexual dysfunction. Sex. Med. Rev. 7 (4), 604–613. https://doi.org/10.1016/j.sxmr.2019.05.005 (2019).
Article PubMed PubMed Central Google Scholar
Musicki, B., Hannan, J. L., Lagoda, G., Bivalacqua, T. J. & Burnett, A. L. Mechanistic link between erectile dysfunction and systemic endothelial dysfunction in type 2 diabetic rats. Andrology 4 (5), 977–983. https://doi.org/10.1111/andr.12218 (2016).
Article CAS PubMed PubMed Central Google Scholar
Download references
All authors thank the participants of the NHANES database.
The Fourth School of Clinical Medicine, Zhejiang Chinese Medical University, Hangzhou First People’s Hospital, Hangzhou, Zhejiang, China
Donggang Shan & Chenze Yan
Department of Hepatobiliary Surgery, Affiliated Hangzhou First People’s Hospital, School of Medicine, Westlake University, Hangzhou, Zhejiang, China
Zhong Jia
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
Donggang, Shan: Writing Original Draft, Visualization, Investigation, Formal AnalysisChenze, Yan: Resources, SupervisionZhong, Jia: Writing – Review & Editing.
Correspondence to Zhong Jia.
The authors declare no competing interests.
The research was examined and approved by the NCHS Ethics Review Board. The participants provided written, informed consent to participate in the NHANES study. The NHANES 2001–2004 was approved by the NCHS Research Ethics Review Board (Protocol #98 − 12). Our study utilized anonymized, publicly available data and did not involve animal or human clinical trials, therefore, it was exempt from additional ethics committee approval. The Ethics Review Committee of Hangzhou First People’s Hospital affiliated to Westlake University Medical School exempted the study.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Reprints and permissions
Shan, D., Yan, C. & Jia, Z. An L-shaped association between lymphocyte-to-monocyte ratio and erectile dysfunction in NHANES 2001–2004. Sci Rep 15, 857 (2025). https://doi.org/10.1038/s41598-025-85261-2
Download citation
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-85261-2
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Advertisement
© 2025 Springer Nature Limited
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
