‘The pandemic clock is ticking,’ one scientist said. ‘We just don’t know what time it is.’
‘The pandemic clock is ticking,’ one scientist said. ‘We just don’t know what time it is.’
‘The pandemic clock is ticking,’ one scientist said. ‘We just don’t know what time it is.’
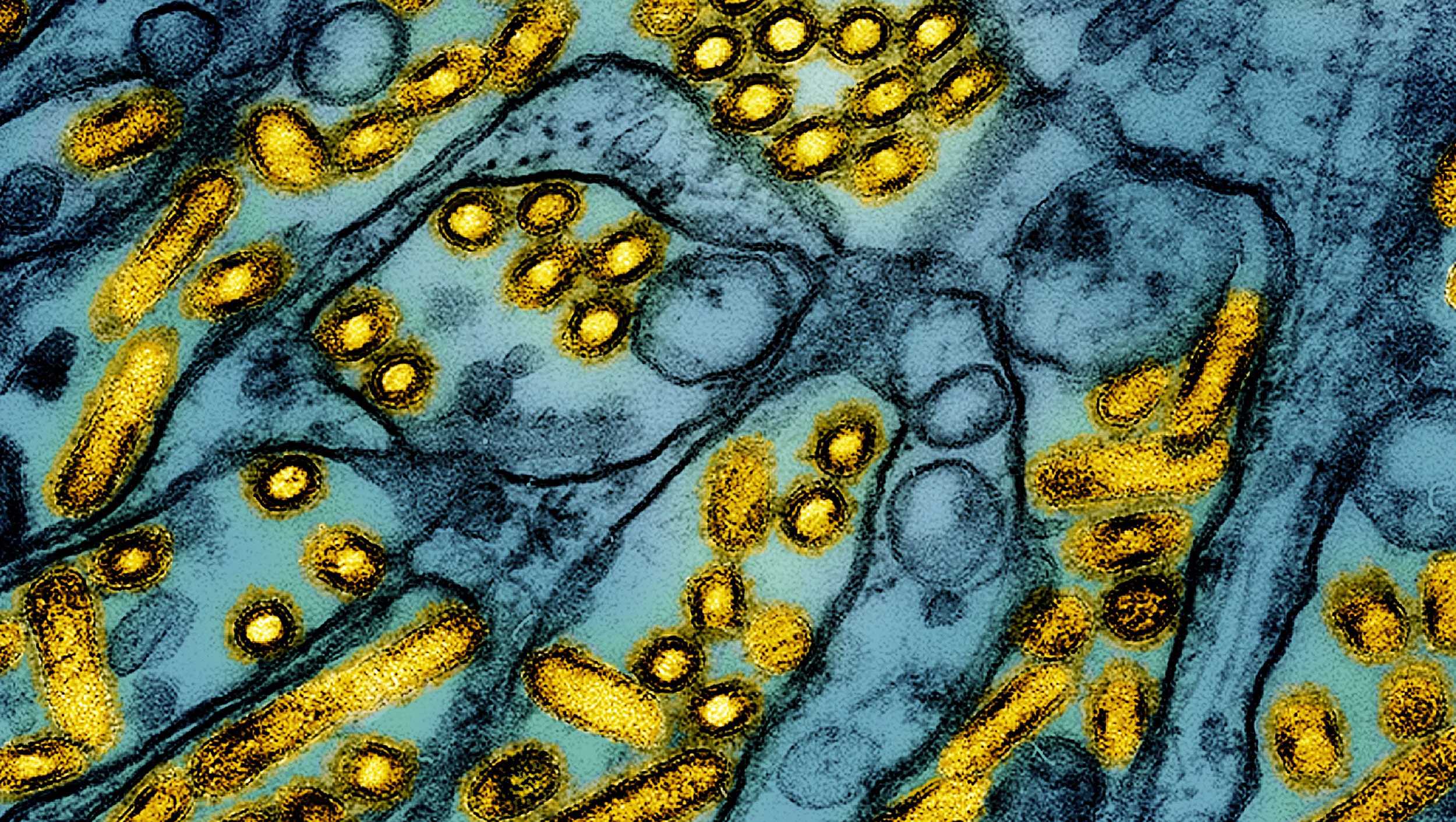
The U.S. hasn’t learned lessons from the COVID-19 pandemic that it could use to mitigate the threat of pathogens like H5N1 bird flu that keep showing signs of their own pandemic potential, health experts told CNN Friday.
Related video above: First severe bird flu case in the US reported
“We kind of have our head in the sand about how widespread this is from the zoonotic standpoint, from the animal-to-human standpoint,” Dr. Deborah Birx, the White House coronavirus response coordinator under President Donald Trump, said on “CNN Newsroom” with Pamela Brown.
Birx called for much wider-spread testing of farm workers who make up the majority of identified cases in the U.S., noting the country is heading into an even higher-risk period as seasonal flu begins to circulate. That raises the possibility a person could get infected with both seasonal flu and H5N1, and the viruses could swap gene segments, Birx said, giving the bird flu virus more tools to better infect humans, a phenomenon known as reassortment.
A spokesperson for the U.S. Centers for Disease Control and Prevention pushed back on Friday, telling CNN in a statement that the “comments about avian flu (H5N1) testing are out of date, misleading and inaccurate.”
“Despite data indicating that asymptomatic infections are rare, CDC changed its recommendations back in November to widen the testing net to include testing asymptomatic people with high-risk exposure to avian flu, and during the summer, it instructed hospitals to continue subtyping flu viruses as part of the nationwide monitoring effort, instead of the normal ramping down of surveillance at the end of flu season,” the spokesperson said.
“The result: more than 70,000 specimens have been tested, looking for novel flu viruses; more than 10,000 people exposed to avian flu have been monitored for symptoms, and 540 people have been tested specifically for H5N1,” the spokesperson continued. “Additionally, CDC partnerships with commercial labs mean that H5N1 tests are now available to doctor’s offices around the country, significantly increasing testing capacity.”
The CDC added it has a seasonal flu vaccination campaign underway for farm workers in states with infected herds to help protect them from seasonal flu and to reduce the chance of reassortment with the H5N1 virus.
The agency has also said there’s currently no human-to-human spread of H5N1. But risks continue to emerge that the virus could evolve to more easily infect people.
The CDC reported Thursday that a genetic analysis of samples from the patient in Louisiana recently hospitalized with the country’s first severe case of H5N1 show the virus likely mutated in the patient to become potentially more transmissible to humans, but there’s no evidence the virus has been passed to anyone else.
The patient was likely infected after having contact with sick and dead birds in a backyard flock, the CDC said earlier this month. In its Thursday analysis, the agency said the mutations it identified in samples taken during the patient’s hospitalization weren’t found in the birds, suggesting they aren’t in the virus widely circulating in wildlife.
The mutations, similar to ones observed in a hospitalized patient in British Columbia, Canada, may make it easier for the virus to bind to cell receptors in humans’ upper respiratory tracts, the CDC said.
“The changes observed were likely generated by replication of this virus in the patient with advanced disease rather than primarily transmitted at the time of infection,” the agency said. “Although concerning, and a reminder that A(H5N1) viruses can develop changes during the clinical course of a human infection, these changes would be more concerning if found in animal hosts or in early stages of infection … when these changes might be more likely to facilitate spread to close contacts.”
The CDC emphasized the risk to the general public has not changed and remains low, but said the detection of the genetic mutations “underscores the importance of ongoing genomic surveillance in people and animals, containment of avian influenza A(H5) outbreaks in dairy cattle and poultry, and prevention measures among people with exposure to infected animals or environments.”
The analysis found no changes associated with markers that might mean antiviral drugs wouldn’t work as well against the virus, the CDC added, and noted the samples are closely related to strains that could be used to make vaccines, if needed.
The sequences also didn’t show changes in genes associated with adaptation to mammals, the CDC found. The patient was infected with a strain known as D1.1 that’s closely related to viruses circulating in wild birds and poultry in the U.S.; another strain known as B3.13 has been spreading widely in dairy cows and hasn’t been found to cause severe disease in humans in the U.S.
“While this sounds like good news, the H5N1 situation remains grim,” Dr. Angela Rasmussen, a virologist at the Vaccine and Infectious Disease Organization at the University of Saskatchewan in Canada, posted on Bluesky on Thursday.
“There has been an explosion of human cases,” she said. “We don’t know what combination of mutations would lead to a pandemic H5N1 virus … but the more humans are infected, the more chances a pandemic virus will emerge.”
The CDC has confirmed 65 cases of H5N1 bird flu in humans in 2024. Of those, 39 were associated with dairy herds and 23 with poultry farms and culling operations. For two cases, the source of exposure is unknown. The severe case in Louisiana is the only one associated with backyard flocks.
Dr. Paul Offit, a vaccine scientist at Children’s Hospital of Philadelphia, noted the CDC said the mutations “may” enable the virus to bind better to cell receptors in humans’ upper respiratory tracts, not that they clearly do.
“I’d like to see clear evidence … that it binds well,” Offit told CNN Friday. “That hasn’t happened yet.”
“And more importantly,” Offit added, “there’s not the clinical relevance that you see human-to-human spread.”
The spread among animals like cows, though, has some health experts on high alert. Since the virus was first found in cattle in March, outbreaks have been detected in herds in 16 states.
This month, the U.S. Department of Agriculture began a national milk testing program to track the spread of the virus through dairy cattle, and the agency has thus far brought on 13 states that account for almost half of the country’s dairy production.
The program requires that raw milk samples be collected before the pasteurization process and shared with USDA for testing.
Government agencies say pasteurization inactivates the virus, making pasteurized milk safe to drink. The Food and Drug Administration and other health agencies warn consumers not to drink raw milk, not just because of the risk of H5N1 but also E. coli, salmonella and listeria.
That the H5N1 virus has already spread so rapidly among cattle, though, suggests “the USDA has basically dropped the ball, big-time,” said Dr. Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota, in an interview with CNN Friday. “I think it was out of fear to protect the industry. And they thought it was going to burn out, and it didn’t.”
Osterholm also said the US and others around the world should have done more to examine lessons from the Covid-19 pandemic, and to accelerate work improving flu vaccines.
And, he noted, “You’ve got the new administration coming and saying they’re going to do in infectious diseases [research] for the next eight years,” referring to comments made by President Trump’s nominee to lead the US Department of Health and Human Services, Robert F. Kennedy, Jr.
Osterholm said his risk assessment for H5N1 hasn’t changed as a result of the Louisiana findings this week, but that he’s always concerned about the threat pathogens like the bird flu virus pose.
“The pandemic clock is ticking,” Osterholm said. “We just don’t know what time it is.”
Hearst Television participates in various affiliate marketing programs, which means we may get paid commissions on editorially chosen products purchased through our links to retailer sites.
