Advertisement
BMC Public Health volume 24, Article number: 3578 (2024)
Metrics details
Although many studies have reported the relationship between female hormone intake and cardiovascular disease (CVD) development, their association has not been fully elucidated and defined, based on data from the Third National Health and Nutrition Examination Survey intending to assess the health and nutritional status of non-institutionalized children and adults in the United States. This study examined the relationship between female hormone intake and coronary artery disease (CVD) development in 38,745 women, averaging 38.10 ± 12.59 years in age. We explored the association between hormone intake and CVD incidence, considering various social determinants of health (SDOH) with statistical methods like Chi-square tests, logistic regression, and stratified Chi-square analysis. Our findings reveal a complex relationship between female hormone intake and CVD development. Hormones appear to reduce CVD risk in women over 60 years old. However, hormone intake correlates with increased CVD risk in highly educated women. Socioeconomic status also influences this relationship; while hormones pose a risk factor for heart failure and stroke in impoverished or wealthy women, they serve as a protective factor against CVD for middle-income women. Additionally, hormonal intake seems beneficial for women who experienced menarche between 13 and 15 years old, menopause between 30 and 49, and had 7–9 pregnancies, especially when coupled with a diet low in sugar, fat, cholesterol, and adequate folic acid intake. These results indicate that while hormones can prevent CVD under specific conditions, their impact can be detrimental in different SDOH contexts. In conclusion, while appropriate hormone intake can prevent CVD, its effects vary across different demographic and health backgrounds. This underscores the necessity for meticulous screening of SDOH factors in clinical settings to maximize the protective benefits of hormones against CVD.
Peer Review reports
Cardiovascular disease (CVD) is a cardiovascular disease caused by reduced blood flow in the coronary arteries, mainly from atherosclerosis. It is often classified into stable or unstable angina and myocardial infarction, which may ultimately lead to heart failure or sudden cardiac death according to the clinical symptoms, depending mainly on the degree of stenosis due to atherosclerosis. It is the leading cause of human death all over the world. In the United States, approximately 20.1 million people have a CVD, and the prevalence is up to 30% among those over 80 years old [1]. The highest percentage of prevalence is in chronic stable angina, with approximately 11.1 million people. Although mortality from CVD has declined by a relative 25% over the past decade as a result of progressive understanding of CVD and advances in medical technology, the total number of deaths has increased, and it remains the leading cause of death in the United States and worldwide [2].
Endocrine and metabolic abnormalities such as hypertension, diabetes, hyperglycemia, obesity, and dyslipidemia are the main modifiable risk factors for CVD [3,4,5]. Moreover, gender, age, and race are associated with the prevalence of CVD [6]. Epidemiological studies found a higher incidence of myocardial infarction among Blacks than Whites in the Atherosclerosis Risk in Communities (ARIC) study in patients aged 65–84 [7]. It reported that the incidence and mortality of CVD in premenopausal women are significantly lower than those of men of the same age, and the incidence and mortality of CVD in postmenopausal women are similar to those of men [8,9,10,11]. It is attributed to the difference in estrogen levels in the premenopausal or postmenopausal period in women, and the main components of estrogen include estradiol, estrone, estriol, and other lipid-soluble steroid hormones, secreted by the ovaries [12, 13]. Estrogen replacement therapy reduces the risk of coronary artery disease in postmenopausal women [14,15,16]. It protects cardiomyocytes, reduces fibroblast collagen, boosts HDL, lowers LDL, and has cardiovascular protective effects [17]. Combined with progestogen therapy to lower lipoprotein A, improve cardiac autonomic control, and prevent aging changes in endothelial function [18]. Estrogen also regulates blood vessel and cell function and is involved in inflammatory responses and metabolism. Estrogen reduces monocyte adhesion through endoplasmic reticulum mechanisms and reduces vascular inflammation [19]. It reduces endothelial cell apoptosis, inhibits smooth muscle cell proliferation and migration, and improves atherosclerosis [20]. High estrogen levels promote Th2 and Treg immune balance and exert anti-inflammatory effects.
Social determinants of health (SDOH) such as race, education, socioeconomic status, housing, medical care, and food significantly impact health. [21]Coronary heart disease is closely related to SDOH and is often overlooked in female hormone and coronary artery disease (CVD) studies [21].Women often face low socioeconomic, educational, stress, diet, and access to health care, resulting in low health resources, which are major confounding factors in CVD studies [14, 15]. Studies have shown that hormone intake is associated with CVD [22], but animal studies cannot directly infer humans [23, 24]. Observational studies have shown that menopausal hormone therapy (MHT) has a positive effect on CVD risk factors and reduces morbidity. However, the results of clinical studies are uncertain due to the neglect of SDOH or the small number of women [25, 26]. Therefore, based on data from the Third National Health and Nutrition Examination Survey (NHANES III) over a 20-year period that included 38,745 cases, our study performed a stratified Chi-square test to accurately assess whether female hormone intake is associated with the development of CVD in women, which rigorously controlled for SDOH status in the included patients. And we aimed to evaluate female hormone intake’s preventive or therapeutic potential in the development of CVD.
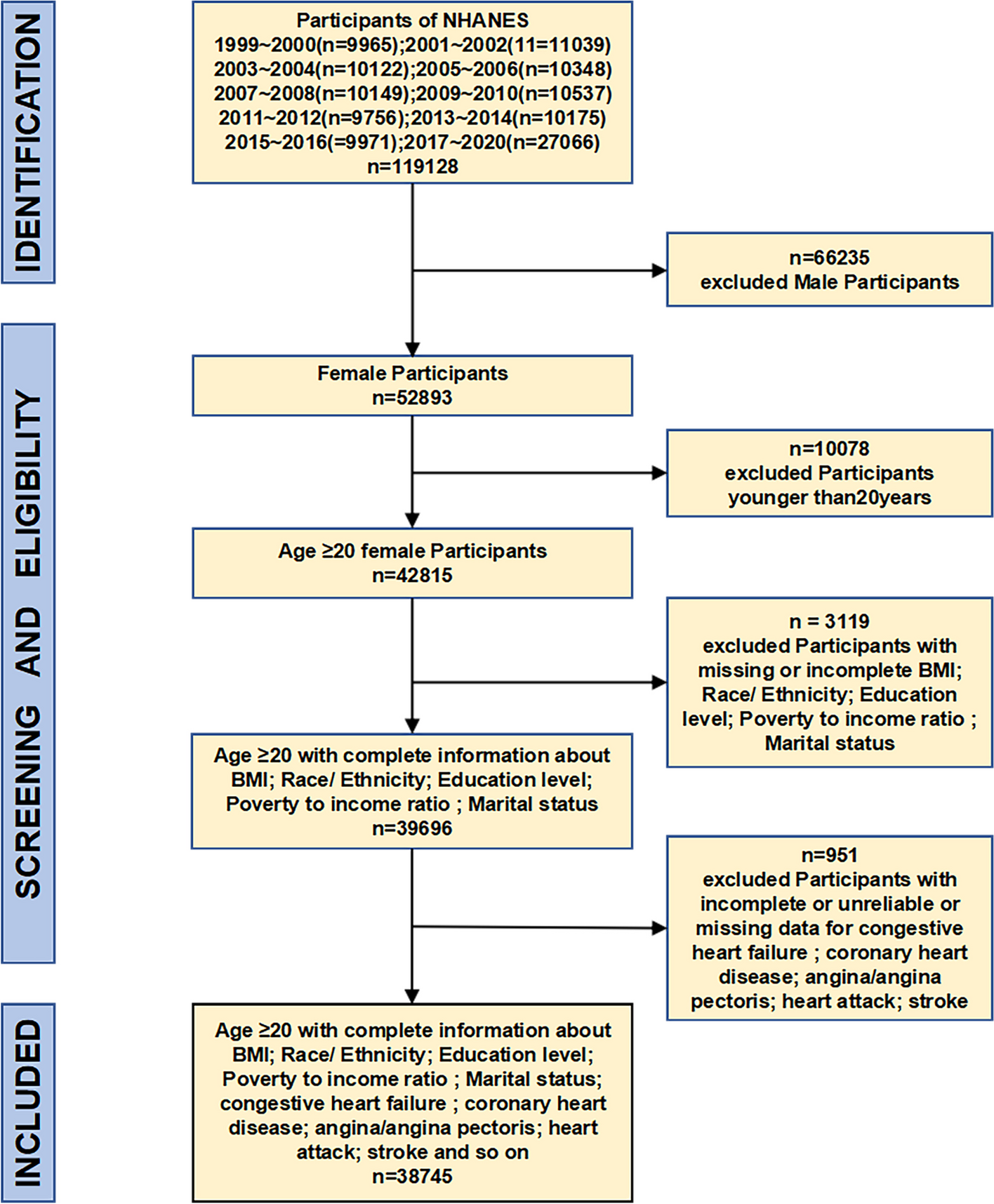
Data came from the third NHANES from 1999 to 2020. NHANES III was a cross-sectional study intended to assess the health and nutritional status of non-institutionalized children and adults in the United States. This survey recorded dietary information and behavior questionnaire for adults and children through family interviews, blood sample collection at the Mobile Examination Center, and a comprehensive physical examination. A total of 119,128 people participated in NHANES 1999 – 2020. This study excluded male participants and participants younger than 20; missing or incomplete socioeconomic factors (education, family income level, and body mass index); and incomplete, unreliable, or uncertain factors related to CVD. Finally, the study included 38,745 eligible participants. Specific study design, sampling, and exclusion criteria are described in Fig. 1. The publicly available data were used, and no ethical approval was involved in this analysis.
Flow chart of the screening process for the selection of participants in NHANES1999–2020
Whether they had CVD was based on their health status in the questionnaire, which included ” Ever told you had congestive heart failure,” ” Ever told you had angina/angina pectoris,” “Ever told you that you had a heart attack,” and “Ever told you that you had a stroke”. According to the answer “yes” or “no” to these questionnaires, we determine whether they have one or more of the above-questioned four clinical features of CVD.
Female participants were asked: “Ever used female hormones such as estrogen and progesterone (include any forms of female hormones, such as pills, cream, patch, and injectables, but do not include birth control methods or use for infertility)?”Additionally, many women take estrogen as a contraceptive, not for any disease treatment. Therefore, when women were asked, “Have you ever taken the pill for any reason.” Their answers were divided into “yes” or “no.” Those who answered “yes” to one or two of the above two questions were classified as taking female hormones. Those who answered “no” to both questions were classified as not taking female hormones.
The Centers for Disease Control and Prevention and the World Health Organization define SDOH as the conditions in the environments where people are born, live, learn, work, play, worship, and age that affects a wide range of health, functioning, and quality of life outcomes and risks from economic, social, environmental, and psychosocial perspectives [27].
SDOH factors included in this study include age, race (Mexican Americans, Non-Hispanic White, Non-Hispanic Black, Others Hispanic or Other races), education level (High school or below, Some College, College graduate or above), family income (Poverty to income ratio ≤ 1.30, Poverty to income ratio between1.31 ~ 3.38, Poverty to income ratio ≥ 3.39), marital status (Married/living with partner or Not married). These SDOH status was based on their answers in the questionnaire, which included “Age in years of the participant at the time of screening. Individuals80 and over are topcoded at 80 years of age.” ” Recode of reported race and Hispanic origin information.” “What is the highest grade or level of school {you have/Sp has} completed or the highest degree {you have/s/he has} received?” “Marital status” and “A ratio of family income to poverty guidelines.”.
The population analyzed in this study was divided into those taking female hormones and those not taking female hormones. Covariates in multivariate models include SDOH factors associated with female hormones, such as age at menarche, menopause, number of pregnancies, diet, and average sleep duration per night, are also covariates. Based on NHANES, each covariant was classified into subgroups for comparison. The detailed classification criteria are provided in Supplementary Table 1.
Chi-square analysis was performed to compare the SDOH characteristics of participants with or without CVD and whether they took the female hormones during home interviews. Multivariate logistic regression was established to define the association between female hormone intake and CVD while adjusting for all covariates. The covariates considered in multivariate models include age, ethnicity, and socioeconomic indicators such as the highest level of education obtained, marital status, income level, and BMI. Moreover, we compared the risk of CVD between participants taking or not taking female hormones in different subgroups of covariates using the Stratified Chi-square test with participants not taking female hormones as reference subjects. The risk of taking female hormones on CVD development was evaluated by odds ratio (OR) and reported by 95% CI with a two-tailed significance level of 0.05. An OR < 1 indicates a protective role of female hormone intake on CVD, and OR > 1 indicates its opposite role. All statistical analyses were performed using SPSS 25.0 with appropriate sampling weights to account for stratification.
We analyze 38,745 eligible female participants with an average age of 38.10 ± 12.59 years old. Table 1 shows the characteristics of all 38,745 female participants. Among them, 35,041 participants (90.44%) without CVD, 3704 participants (9.56%) have CVD, 1356 cases (3.50%) with congestive heart failure, 1278 cases (3.30%) with angina/angina pectoris, 1511 (3.90%) with heart attack, 1007 patients (2.60%) with stroke.
The correlation analysis shows that the SDOH factors, including age, ethnicity, education level, poverty to income ratio, and marital status, are associated with CVD (Table 1, p-values < 0.001). Higher age is significantly associated with CVD prevalence, presented in any clinical feature ( CVD + vs. CVD-: congestive heart failure: 41.61 ± 5.99 vs. 34.94 ± 9.47; angina/angina pectoris 42.53 ± 9.61 vs. 34.96 ± 9.46; heart attack: 41.85 ± 6.84 vs. 34.95 ± 9.47; stroke:40.61 ± 8.54 vs. 34.93 ± 9.46). The participants of the non-Hispanic white race are less likely to get CVD, specifically in heart attack (31.7% vs. 34.8%) and stroke (33.3% vs 34.7%). In contrast, non-Hispanic Blacks is prone to get CVD (congestive heart failure: 31.0% vs. 27.3%; angina/angina pectoris 38.1% vs. 26.9%; heart attack: 41.5% vs. 26.5%; stroke:29.4% vs. 27.2%). The proportion of participants in poverty with the four clinical manifestations of CVD is lower than those out of poverty (p-values < 0.001). Among the factors affecting female hormone levels, those who have experienced Bilateral Ovariectomy and Arthritis have a higher prevalence of four clinically manifested symptoms of CVD. The majority of CVD is generally higher among those who have been pregnant more than six times. The age at menarche < 10 or ≥ 16 years old and at menopause < 30 years or ≥ 60 years are associated with a higher prevalence of CVD. And there are fewer participants with CVD among obese participants (BMI ≥ 30). Additionally, the proportion of participants who intake female hormones which get CVD is significantly lower than those without CVD (congestive heart failure: 63.6% vs. 73.7%; angina/angina: 59.8% vs. 73.7%%; heart attack:66.7% vs. 73.7%; stroke:73.9% vs. 74.6%).
Table 2 summarizes the analysis results for the association of the other characteristics and female hormones intake status of the participants. 71.9% of adult women have taken female hormones, and compared with women who didn’t accept female hormones, the participants who take female hormones were younger (49.38 ± 9.42y vs. 51.02 ± 8.61y, p-values < 0.001) as well as high-income (34.7% vs. 19.8%, p-values < 0.001); The married women are inclined to take the female hormones (59.3% vs. 47.1%, p-values < 0.001).
The multiple logistic regression analysis was used to analyze of the association between CVD and female hormone intake before and after adjustment for covariates (Fig. 2 and Table 3). In multiple regression analysis, female hormone intake was a risk factor before adjusting for covariates, for congestive heart failure (OR = 1.563, 95%CI:1.557–1.570), angina pectoris/angina pectoris (OR = 1.398, 95%CI:1.391–1.406), heart attack (OR = 1.102, 95%CI:1.097–1.107), and stroke (OR = 1.026, 95%CI: 1.022–1.029). After adjusting for all covariates we included (Model15), intake of female hormone seemed to be a protective factor of congestive heart failure (OR = 0.892, 95%CI: 0.890–0.894); Angina/angina pectoris (OR = 0.782, 95%CI:0.780–0.784); heart attack (OR = 0.963, 95%CI:0.959–0.967) and stroke (OR = 0.942, 95%CI:0.934–0.950). These results suggest that intake of female hormone plays a protective role in CVD.
The logistic regression analysis of the association between CVD and female hormone intake before and after adjustment for covariates. A congestive heart failure (B) angina/angina pectoris (C) heart attack (D) stroke
Additionally, we categorized 12,808 women based on their menopausal status. Table 4 details the multiple logistic regression analysis evaluating the correlation between coronary artery disease (CVD) and pre- and post-menopausal hormone intake, with adjustments for covariates. The covariates included in our multiple regression analyses were race, age, education level, marital status, poverty to income ratio, age at menarche, age at menopause, and number of pregnancies. Post-adjustment, hormone intake was found to be a protective factor against CVD, as indicated by the odds ratios for congestive heart failure (OR = 0.915, 95% CI: 0.846–0.990), angina/angina pectoris (OR = 0.915, 95% CI: 0.849–0.986), heart attack (OR = 0.757, 95% CI: 0.687–0.834), and stroke (OR = 0.832, 95% CI: 0.768–0.901). These findings underscore the protective effect of female hormone intake on the development of CVD in postmenopausal women.
To accurately assess the effect of hormone-related factors on taking female hormones and the occurrence of CVD, we make a stratified analysis for the included covariates by using age, education level, household economic level, BMI, endogenous female hormone levels, and dietary and metabolic levels as stratification variables (Table 5). The number of female respondents with female hormone intake aged ≥ 60 years old who suffered from CVD is less than those who did not suffer from CVD. Conversely, women aged between 40–60 years old who take in female hormones are at an elevated risk of a heart attack.
Additionally, taking female hormones poses a stroke risk related to menopause duration < 10 or ≥ 10 years. However, for women with a shorter duration of menopause (< 10), taking female hormones may make them less susceptible to developing heart failure, heart attacks and angina. In contrast, for women with a longer duration of menopause (≥ 10), the risk of these conditions is higher. Interestingly, for women who received higher levels of education (college graduates or above), the probability of female hormone intake in people with angina pectoris, heart attack and stroke is more than those without angina pectoris, heart attack and stroke. While the probability of female hormone intake in women with CVD is less than in women without CVD under lower education levels. However, women at the middle-income level who take in female hormones are prone to suffer any type of CVD. Moreover, the women with menarche at 13–15 years old, menopause at 30–49 years old, and pregnancies 7–9 times, as well as with a low-sugar (< 25 g/day), low-fat (< 50 g/day), low-cholesterol diet (< 300 mg/day) and proper folic acid intake (> 800 ug/day) intake female hormones have a protective effect on the development of CVD (p-values < 0.001). These results suggest that the intake of female hormones is a protective or risk factor for CVD, depending on the different SODH factors and the factors that affect the endogenous estrogen release level.
Although the protective effect of female hormones on CVD has been demonstrated in animal experiments [23, 24], with the emergence and development of gender medicine, it has been gradually recognized that the SDOH factors exert a binding effect on many disease occurrences [28]. Therefore, the relationship between the occurrence of CVD and female hormones intake could not be accurately defined through previous clinical trials [15]. Therefore, this study assessed the relation between female hormone intake and the development of CVD in 38,745 eligible female participants, based on data from the NHANS III over 20 years, and demonstrated that intake of female hormones is a protective or risk factor for the occurrence of the CVD depending on the different SODH factor statues and the related factors that affect the endogenous estrogen release level.
Correlation analysis found that the occurrence of four clinical manifestations of CVD in females is significantly related to SDOH factors (age, race, education level, family income, and marital status) and the other factors that affect endogenous hormone release levels (bilateral ovariectomy, pregnancies number, menarche age, menopause age), and exogenous hormone intake. In addition, exogenous hormone intake in women, including female hormones for therapeutic purposes and contraceptives, was associated with many demographic and endocrine factors. Thus, these factors act as confounders that influence the exact relationship between female hormones and CVD. Furthermore, logistic regression analysis showed that female hormone intake was a risk factor for CVD development without adjusting for covariates. After adjusting for race, age, education level, marital status, family economic status, age at menarche and menarche, and the number of pregnancies, the female hormone intake shifts to a protective factor for CVD development. In future clinical studies, investigators should consider various demographic and endocrine factors affecting female hormone levels.
We found several interesting results in the stratified analysis of covariates. First, it showed that female hormone intake reduces the risk of the four clinical features of CVD in women aged ≥ 60 years old, but it increases the risk of a heart attack in women between 40–60 years old and angina pectoris and stroke in women aged between 20–40 years old. It suggests that exogenous estrogen supplementation can prevent CVD in old females with lower levels of estrogen (women aged ≥ 60 years old). A prospective cohort study found that bilateral oophorectomy increased the risk of CVD, while estrogen replacement therapy could reverse this condition [29].In addition, computed tomography scanning of coronary artery calcification revealed a lower prevalence of plaque in coronary arteries in patients with estrogen replacement therapy within five years of oophorectomy [30].
Interestingly, for women who received higher levels of education (college graduates or above), intake of female hormones is a risk factor for CVD, while it is a protective factor for CVD in women with lower education levels. It may attribute to females with high education levels who are often engaged in mental work and less physical activity. A possible explanation is that women with high levels of education are primarily engaged in mental work. They have much sedentary time due to their occupational characteristics (including TV watching, computer use, and driving).Studies have shown that passive activity is associated with an increased risk of cardiovascular disease and all-cause mortality [20], meaning that the reduction in physical work due to sedentary activity which is a significant factor in the incidence of CVD.
Attractively, for women in poverty (poverty to income ratio ≤ 1.3) or in wealthy (poverty to income ratio ≥ 3.39), female hormone intake is a risk factor for congestive heart failure and stroke, but it is a protective factor for the four clinical features of CVD for women in middle-income level. Many studies reported that poverty and socioeconomic disadvantage in low-income communities are significant risk factors for developing coronary artery disease [31,32,33,34]. Moreover, these studies only dichotomized economic levels into the poor and non-poor groups. Adam L. Beckman et al. found an increased prevalence of dyslipidemia and obesity in the high and low PIR groups. One study classified economic levels into high, moderate, and low PIR and found an increased prevalence of dyslipidemia and obesity in the high and low PIR groups [35], and the investigated symptoms are close to CVD. In addition, studies also have suggested that low income leads to a higher prevalence of central obesity, sedentary, and smoking [36]. However, some studies have attributed this phenomenon to the psychological stress of people in poverty rather than specific income [37]. Poverty as a chronic stressor leads to physiological dysregulation of the responsiveness to stress through the hypothalamic–pituitary–adrenal (HPA) axis and the sympathetic nervous system (SNS) [38, 39], which are associated with an increased cardiometabolic risk and for affluent people, they may be equally exposed to psychological problems [40] such as obesity, sedentary lifestyle, smoking, and especially anxiety and depression [41,42,43], leading to an increased risk of CVD.
Moreover, the factors affecting endogenous estrogen secretion levels can lead to the positive or negative effects of taking female hormones on the development of CVD. The women of menarche at 13–15 years old, menopause at 30–49 years old, and pregnancies 7–9 times, as well as with a low-sugar (< 25 g/day), low-fat (< 50 g/day), low-cholesterol diet (< 300 mg/day) and proper folic acid intake (> 400 ug/day) intake female hormones have a protective effect on the development of CVD. And the opposite of these factors can lead to the unbeneficial result of taking female hormones to CVD occurrence. These results suggest that an intake of female hormones is a protective or risk factor for CVD, depending on the different SODH factors that affect the endogenous estrogen release level. Mainly in women with older age (≥ 60 years old) and low educational level, in poverty or wealth, with menarche aged at 13–15 years old, menopause age at 30–49 years old, and with a low sugar and fat diet. It explains the contradictory results of many clinical studies. The limited sample size makes it impossible to stratify the study population in detail and obtain more accurate analysis results.
The findings of this study hold significant implications for clinical practice and public health strategies. Initially, they underscore the necessity for personalized medicine, emphasizing the need for tailored hormone replacement therapy (HRT) based on the specific social determinants of health (SDOH) in women, which can determine the risk of CVD from taking female hormones and make individualized decisions about timing and dosage adjustments. For instance, HRT may serve as a preventative measure for CVD in women over the age of 60. Instead, Women with certain characteristics should make more cautious decisions when using exogenous hormones, such as younger age, higher education, poor or excessive economic situation, and poor dietary conditions and habits. Furthermore, considering lifestyle factors in women with higher educational attainment is also essential, as these factors may influence the cardiovascular effects of HRT. Public health professionals can utilize this information to design and implement targeted educational and preventive programs to raise awareness among women about risk factors for CVD and to encourage healthy lifestyle choices.
Additionally, the study’s findings reveal the relationship between socioeconomic status and CVD risk, suggesting that policymakers should address the specific health needs of women from low-income and high-income communities, potentially providing increased support and resources for these groups. For example, the US Healthy People 2030 agenda [44] addresses SDOH factors contributing to health inequalities. Moreover, the results indicate that proper dietary and nutritional intake, such as a low-sugar, low-fat, low-cholesterol diet, and adequate folic acid intake, may be associated with the protective effects of female hormone intake. This provides clinicians with guidance on promoting healthy dietary habits, which could contribute to reducing the risk of CVD.
The advantage of this study is that the NHANES III database has many nationwide cross-sectional study samples, which can represent the overall American population after weighing the samples. Therefore, the potential factors that may affect the relationship of exposure factors to outcome variables included in this study are relatively comprehensive. Additionally, we made a stratified analysis to precisely define the protective or risk role of female hormone intake for the development of CVD among subgroup populations with different SDOH backgrounds. Moreover, selection bias can be avoided as the sample data comes from community questionnaires. However, there some limitations still existed in this study. Firstly, NHANES III used a self-reported questionnaire to inquire about female hormone intake, which introduces recall and self-reported bias; Secondly, the data comes from cross-sectional studies, which means that further prospective studies are needed to verify the causal relationship between female hormones and CVD.
Our study concludes that various SDOH factors that affect hormone secretion levels are significantly associated with the development of CVD. And they are also associated with whether female hormones were taken or not. Therefore, exogenous administration of female hormones has a preventive effect on the occurrence of CVD in specific groups of women. Furthermore, our results suggest that female hormone intake is a protective or risk factor for CVD, depending on the factors affecting the endogenous estrogen release level. Therefore, comprehensive and systematic consideration of various factors affecting endogenous hormone secretion levels is significant for whether female patients can obtain positive clinical benefits by taking female hormones in clinical application.
More information about the NHANES could be obtained at: http://www.cdc.gov/nhanes.
Coronary artery disease
Atherosclerosis Risk in Communities
High-density lipoprotein
Low-density lipoprotein
Sociocultural determinants of health
The Third National Health and Nutrition Examination Survey
Body mass index
Diabetes Mellitus
Coronary heart disease
Odds ratio
Confidence interval
Power impact ratio
Renin-angiotensin-aldosterone
Virani SS, Newby LK, Arnold SV, et al. 2023 AHA/ACC/ACCP/ASPC/NLA/PCNA Guideline for the Management of Patients With Chronic Coronary Disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2023;82(5):833–955.
PubMed Google Scholar
Mensah GA, Fuster V, Roth GA. A heart-healthy and stroke-free world: using data to inform global action. J Am Coll Cardiol. 2023;82(6):2343–9.
PubMed Google Scholar
Wolf D, Ley K. Immunity and inflammation in atherosclerosis. Circ Res. 2019;124(10):315–27.
CAS PubMed PubMed Central Google Scholar
Mone P, Gambardella J, Minicucci F, et al. Hyperglycemia drives stent restenosis in STEMI patients. Diabetes Care. 2021;44(2):e192–3.
PubMed PubMed Central Google Scholar
Cui K, Fu R, Yang J, et al. Admission blood glucose and 2-year mortality after acute myocardial infarction in patients with different glucose metabolism status: a prospective, nationwide, and multicenter registry. Front Endocrinol (Lausanne). 2022;13(8):898384.
PubMed Google Scholar
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(7):2935–59.
PubMed Google Scholar
Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the american heart association. Circulation. 2017;135(10):e146–603.
PubMed PubMed Central Google Scholar
Vogel B, Acevedo M, Appelman Y, et al. The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet. 2021;397(10):2385–438.
PubMed Google Scholar
Hellgren T, Blöndal M, Jortveit J, et al. Sex-related differences in the management and outcomes of patients hospitalized with ST-elevation myocardial infarction: a comparison within four European myocardial infarction registries. Eur Heart J Open. 2022;2(9):oeac042.
PubMed PubMed Central Google Scholar
Singh P, Covassin N, Marlatt K, et al. Obesity, body composition, and sex hormones: implications for cardiovascular risk. Compr Physiol. 2021;12(6):29C49–2993.
Google Scholar
Bots SH, Peters SAE, Woodward M. Sex differences in coronary heart disease and stroke mortality: a global assessment of the effect of ageing between 1980 and 2010. BMJ Glob Health. 2017;2(4):e000298.
PubMed PubMed Central Google Scholar
Blank EW, Wong PY, Lakshmanaswamy R, et al. Both ovarian hormones estrogen and progesterone are necessary for hormonal mammary carcinogenesis in ovariectomized ACI rats. Proc Natl Acad Sci U S A. 2008;105(10):3527–32.
CAS PubMed PubMed Central Google Scholar
Nilsson S, Mäkelä S, Treuter E, et al. Mechanisms of estrogen action. Physiol Rev. 2001;81(6):1535–65.
CAS PubMed Google Scholar
Cho L, Kaunitz AM, Faubion SS, et al. Rethinking menopausal hormone therapy: for whom, what, when, and how long? Circulation. 2023;147(3):597–610.
PubMed PubMed Central Google Scholar
Oliver-Williams C, Glisic M, Shahzad S, et al. The route of administration, timing, duration and dose of postmenopausal hormone therapy and cardiovascular outcomes in women: a systematic review. Hum Reprod Update. 2019;25(9):257–71.
CAS PubMed Google Scholar
Robinson GA, Peng J, Peckham H, et al. Sex hormones drive changes in lipoprotein metabolism. iScience. 2021;24(4):103257.
CAS PubMed PubMed Central Google Scholar
Kararigas G, Bito V, Tinel H, et al. Transcriptome characterization of estrogen-treated human myocardium identifies myosin regulatory light chain interacting protein as a sex-specific element influencing contractile function. J Am Coll Cardiol. 2012;59(6):410–7.
CAS PubMed Google Scholar
Shlipak MG, Simon JA, Vittinghoff E, et al. Estrogen and progestin, lipoprotein(a), and the risk of recurrent coronary heart disease events after menopause. JAMA. 2000;283(3):1845–52.
CAS PubMed Google Scholar
Gordon JL, Rubinow DR, Watkins L, et al. The effect of perimenopausal transdermal estradiol and micronized progesterone on markers of risk for arterial disease. J Clin Endocrinol Metab. 2020;105(2):e2050–2060.
PubMed Google Scholar
Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2023 update: a report from the american heart association. Circulation. 2023;147(2):e93–621.
PubMed Google Scholar
Krzyzanowski MC, Ives CL, Jones NL, et al. The PhenX toolkit: measurement protocols for assessment of social determinants of health. Am J Prev Med. 2023;65(4):534–42.
PubMed PubMed Central Google Scholar
Cislaghi B, Bhatia A, Hallgren EST, et al. Gender norms and gender equality in full-time employment and health: a 97-country analysis of the world values survey. Front Psychol. 2022;13(7):689815.
PubMed PubMed Central Google Scholar
Du M, Shan J, Feng A, et al. Oestrogen receptor β activation protects against myocardial infarction via notch1 signalling. Cardiovasc Drugs Ther. 2020;34(3):165–78.
CAS PubMed PubMed Central Google Scholar
White-Williams C, Rossi LP, Bittner VA, et al. Addressing social determinants of health in the care of patients with heart failure: a scientific statement from the American heart association. Circulation. 2020;141(5):e841–63.
PubMed Google Scholar
Suman S, Pravalika J, Manjula P, et al. Gender and CVD- does it really matters? Curr Probl Cardiol. 2023;48(1):101604.
PubMed Google Scholar
Mital R, Bayne J, Rodriguez F, et al. Race and ethnicity considerations in patients with coronary artery disease and Stroke: JACC Focus Seminar 3/9. J Am Coll Cardiol. 2021;78(5):2483–92.
PubMed Google Scholar
Pourat N, Chen X, Lu C, et al. The relative contribution of social determinants of health among health resources and services administration-funded health centers. Popul Health Manag. 2022;25(7):199–208.
PubMed Google Scholar
Regitz-Zagrosek V, Gebhard C. Gender medicine: effects of sex and gender on cardiovascular disease manifestation and outcomes. Nat Rev Cardiol. 2023;20(10):236–47.
PubMed Google Scholar
Colditz GA, Willett WC, Stampfer MJ, et al. Menopause and the risk of coronary heart disease in women. N Engl J Med. 1987;316(2):1105–10.
CAS PubMed Google Scholar
Allison MA, Manson JE, Langer RD, et al. Oophorectomy, hormone therapy, and subclinical coronary artery disease in women with hysterectomy: the Women’s Health Initiative coronary artery calcium study. Menopause. 2008;15(1):639–47.
PubMed PubMed Central Google Scholar
Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(5):99–106.
CAS PubMed Google Scholar
Nordstrom CK, Diez Roux AV, Jackson SA, et al. The association of personal and neighborhood socioeconomic indicators with subclinical cardiovascular disease in an elderly cohort. The cardiovascular health study. Soc Sci Med. 2004;59(9):2139–47.
PubMed Google Scholar
Auer JW, Berent R, Eber BC. Low socioeconomic status and coronary artery disease. Lancet. 2002;359(7):979–80.
PubMed Google Scholar
He J, Zhu Z, Bundy JD, et al. Trends in cardiovascular risk factors in us adults by race and ethnicity and socioeconomic status, 1999–2018. JAMA. 2021;326(3):1286–98.
PubMed PubMed Central Google Scholar
Beckman AL, Herrin J, Nasir K, et al. Trends in cardiovascular health of US adults by Income, 2005–2014. JAMA Cardiol. 2017;2(5):814–6.
PubMed PubMed Central Google Scholar
Ali MK, Bullard KM, Beckles GL, et al. Household income and cardiovascular disease risks in U.S. children and young adults: analyses from NHANES 1999–2008. Diabetes Care. 2011;34(5):1998–2004.
PubMed PubMed Central Google Scholar
Sullivan S, Kelli HM, Hammadah M, et al. Neighborhood poverty and hemodynamic, neuroendocrine, and immune response to acute stress among patients with coronary artery disease. Psychoneuroendocrinology. 2019;100(8):145–55.
CAS PubMed Google Scholar
Hajat A, Moore K, Do DP, et al. Examining the cross-sectional and longitudinal association between diurnal cortisol and neighborhood characteristics: evidence from the multi-ethnic study of atherosclerosis. Health Place. 2015;34(9):199–206.
PubMed PubMed Central Google Scholar
Lê-Scherban F, Brenner AB, Hicken MT, et al. Child and adult socioeconomic status and the cortisol response to acute stress: evidence from the multi-ethnic study of atherosclerosis. Psychosom Med. 2018;80(7):184–92.
PubMed PubMed Central Google Scholar
Chida Y, Steptoe A. Greater cardiovascular responses to laboratory mental stress are associated with poor subsequent cardiovascular risk status: a meta-analysis of prospective evidence. Hypertension. 2010;55(3):1026–32.
CAS PubMed Google Scholar
Ruscio AM, Hallion LS, Lim CCW, et al. Cross-sectional comparison of the epidemiology of DSM-5 generalized anxiety disorder across the globe. JAMA Psychiat. 2017;74(3):465–75.
Google Scholar
Greenage M, Kulaksizoglu B, Cilingiroglu M, et al. The role of anxiety and emotional stress as a risk factor in treatment-resistant hypertension. Curr Atheroscler Rep. 2011;13(4):129–31.
PubMed Google Scholar
Bhasin SK, Sharma R, Saini NK. Depression, anxiety and stress among adolescent students belonging to affluent families: a school-based study. Indian J Pediatr. 2010;77(2):161–5.
PubMed Google Scholar
U.S. Department of Health and Human Services: Office of Disease Prevention and Health Promotion–Healthy People 2010. Nasnewsletter. 2000;15(3):3.
Download references
Not applicable.
This work was supported by the National Natural Science Foundation of China (Grant No. 82202297) and the Natural Science Basic Research Program of Shaanxi Province (Grant No. 2022JQ-914).
Shenao Qu and Zhixuan Zhang contributed equally to this work.
Center for Regenerative and Reconstructive Medicine, Med-X Institute of Western China Science and Technology Innovation Harbour, First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, 710049, China
Shenao Qu, Zhixuan Zhang, Ran Ju, Yi Lv & Nana Zhang
National Local Joint Engineering Research Center for Precision Surgery and Regenerative Medicine, First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, 710061, China
Shenao Qu, Zhixuan Zhang, Ran Ju, Zhuoqun Li, Xuan Han, Yi Lv & Nana Zhang
Shaanxi Provincial Center for Regenerative Medicine and Surgical Engineering Research Center, First Affiliated Hospital of Xi’an Jiaotong University, No.277, West Yanta Road, Yanta District, Xian, Shaanxi Province, 710061, China
Shenao Qu, Zhixuan Zhang, Ran Ju, Zhuoqun Li, Xuan Han, Yi Lv & Nana Zhang
Department of Thoracic Surgery, Peking University People’s Hospital, Beijing, 100044, China
Zhixuan Zhang
Department of Hepatobiliary Surgery and Institute of Advanced Surgical Technology and Engineering, First Affiliated Hospital of Xi’an Jiaotong University, Xian, 710061, China
Zhuoqun Li, Xuan Han & Yi Lv
Xi’an Jiaotong University Health Science Center, Xi’an, 710061, China
Jing Leng, Zihan Xue & Shiran Tao
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
You can also search for this author in PubMed Google Scholar
All authors contributed to this manuscript. SAQ and ZXZ collected and analyzed the related data and helped draft the manuscript. RJ, ZQL, and JL helped assess analytical methods and reconcile analytical results. XH, XZH, and SRT helped extract the original data. NNZ and YL designed the study, modified the manuscript, and funded this study. All authors read and approved the final manuscript.
Correspondence to Yi Lv or Nana Zhang.
This research analyzed de-identifed information downloaded from the National Health and Nutrition Examination Survey public database. The National Center for Health Statistics Ethics Review Committee granted ethics approval. All methods were carried out in accordance with relevant guidelines and regulations (declaration of Helsinki). All individuals provided written informed consent before participating in the study.
Not applicable.
The authors declare no competing interests.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
Reprints and permissions
Qu, S., Zhang, Z., Ju, R. et al. Association between the female hormone intake and cardiovascular disease in the women: a study based on NHANES 1999–2020. BMC Public Health 24, 3578 (2024). https://doi.org/10.1186/s12889-024-21001-x
Download citation
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-21001-x
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Advertisement
ISSN: 1471-2458
By using this website, you agree to our Terms and Conditions, Your US state privacy rights, Privacy statement and Cookies policy. Your privacy choices/Manage cookies we use in the preference centre.
© 2024 BioMed Central Ltd unless otherwise stated. Part of Springer Nature.
